Focal Fatty Infiltration in the Head of the Pancreas: Evaluation With Multidetector Computed Tomography With Multiplanar Reformation Imaging
Kawamoto, Satomi MD*; Siegelman, Stanley S. MD*; Bluemke, David A. MD, PhD*; Hruban, Ralph H. MD†; Fishman, Elliot K. MD*
Author Information
*The Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins Hospital, Baltimore, MD.
†Department of Pathology, The Sol Goldman Pancreatic Cancer Research Center, Johns Hopkins Hospital, Baltimore, MD.
Received for publication September 13, 2007; accepted October 1, 2007.
Reprints: Satomi Kawamoto, MD, Department of Radiology, Johns Hopkins Hospital, JHOC 3140B, 601 North Caroline Street, Baltimore, MD 21287 (e-mail: [email protected]).
Abstract | |||||||
Fatty infiltration of the pancreas is generally a diffuse process; however, it may be unevenly distributed in the pancreas. Focal fatty infiltration of the pancreas is usually most prominent in the anterior aspect of the head of the pancreas and seen as a region of decreased attenuation on computed tomography and may simulate pancreatic neoplasm. We discuss and illustrate the various features of focal fatty infiltration of the pancreas on multidetector row helical computed tomography with multiplanar reformation images and show how this imaging modality helps to differentiate between focal fatty infiltration of the pancreas and actual pancreatic tumors. | |||||||
Fatty infiltration of the pancreas is relatively common condition and is often incidentally identified on abdominal computed tomographic (CT) scans.1 Fatty infiltration is also known as adipose atrophy, fatty replacement, and lipomatosis of the pancreas.2-4 Fatty infiltration of the pancreas is generally a diffuse process occurring uniformly throughout the gland and occurs most frequently in the elderly and obese populations.1,3 However, fatty infiltration may be unevenly distributed in the pancreas and can be confined to 1 region of the pancreas (focal fatty infiltration).5-10 Similarly, fatty infiltration may spare regions of the pancreas (focal fatty sparing)that is analogous to focal fatty spearing in the liver.11,12 The sonographic,5,6,9,11 CT,7,10-12 and magnetic resonance imaging (MRI) findings 7,8,11 of focal fatty infiltration and focal fatty sparing of the pancreas have been described in the literature. | |||||||
Focal fatty infiltration can mimic a hypoattenuating mass on CT examinations,7 and fatty sparing of the pancreatic head can appear as a "pseudomass."12 These are both normal variants and should not be confused with a neoplasm or other pathological processes. Alternatively, hypoattenuating neoplasms in the pancreatic head should not be mistaken as focal fatty infiltration. | |||||||
The objectives of this article are to discuss and illustrate the CT appearance of focal fatty infiltration in the pancreas that may simulate a hypoattenuating mass and to discuss CT findings to help to differentiate focal fatty infiltration from a pancreatic neoplasm. A brief discussion of the pathological and clinical features of pancreatic fatty infiltration, and possible causes of focal fatty infiltration, including embryological background of the pancreas, are included. The usefulness of MRI to detect and characterize focal fatty infiltration of the pancreas is also briefly discussed. | |||||||
PATHOLOGICAL AND CLINICAL FEATURES OF PANCREATIC FATTY INFILTRATION | |||||||
Macroscopic features of pancreatic fatty infiltration include an increased amount of fat between normal-appearing lobules of pancreatic parenchyma. The gland itself is normal-sized or enlarged, and it often maintains its usual shape and lobular architecture.13 Microscopically, more fat cells are seen in the pancreatic parenchyma.3 There can be a loss of acinar parenchyma, but the islets of Langerhans are usually not affected by fatty infiltration.4 | |||||||
Diffuse mild fatty infiltration of the pancreas is usually of little clinical importance.7 However, an extreme degree of fatty infiltration of the pancreas may be associated with severe exocrine pancreatic insufficiency.4,13 Replacement of pancreatic acini by adipose tissue may lead to exocrine pancreatic insufficiency, with resulting maldigestion of nutrients and a clinical picture of chronic diarrhea, steatorrhea, and weight loss without abdominal pain or diabetes.13 | |||||||
POSSIBLE CAUSES OF FATTY INFILTRATION OF THE PANCREAS | |||||||
Although no single cause has been established for fatty infiltration of the pancreas, it occurs most frequently in the elderly and obese populations.3 It has also been associated with diabetes mellitus, chronic pancreatitis, hepatic disease, dietary deficiency, viral infection, steroid therapy, and obstruction of the pancreatic duct.4 Fatty infiltration of the pancreas may be reversible in patients if they lose weight 14 and in patients with Cushing syndrome or steroid therapy.15 Fatty infiltration of the pancreas has been also reported in advanced cases of cystic fibrosis.15,16 Shwachman syndrome and Johanson-Blizzard syndrome are rare disorders that are associated with exocrine pancreatic insufficiency and fatty replacement of pancreatic parenchyma in children.17 | |||||||
Uneven fatty infiltration may be caused by differences in the histological characteristics between the 2 embryological pancreatic buds.6,9-11 The pancreas forms from 2 separate buds: the dorsal and the ventral buds of endodermal cells arise from the foregut. The dorsal bud originates a short distance above the ventral bud and grows into the dorsal mesentery. The ventral bud arises in conjunction with the developing common bile duct, close to the junction of the foregut with the midgut. Fusion of these 2 buds forms the final pancreas. The ventral bud forms the posterior parts of the head and the upper two thirds or all of the uncinate process; the larger dorsal bud forms the body, tail, and anterior part of the head.18,19 | |||||||
The pancreatic parenchyma that develops from the ventral bud contains smaller and more closely packed lobules and may allow for the macroscopic differentiation of the 2 buds in some cases.19 Microscopically, the embryological dorsal pancreas can be differentiated from the embryological ventral pancreas by less compact, loose lobules of pancreatic parenchyma with larger amount of intralobular adipose tissue compared with the embryological ventral pancreas.5,18-21 | |||||||
Fatty infiltration of the pancreas has also been reported in patients with obstruction of the pancreatic duct due to intraductal calculus or a tumor 4,22,23 and in animal models with ligation of the pancreatic duct.2,24 In patients with focal fatty infiltration due to obstruction of the pancreatic duct, fatty infiltration is more intense upstream from the obstruction.4,12,22 | |||||||
CT TECHNIQUE | |||||||
Computed tomographic examinations were performed on multidetector-row CT scanners, including Siemens Sensation 16 and 64 scanners (Siemens Medical Solutions, Malvern, Pa). Detector collimation settings of 16 × 0.75 or 64 × 0.6 mm were used. The data were reconstructed at 0.75-mm slice thickness at 0.5-mm intervals for multiplanar reformation imaging. For diagnostic reading, 3- or 5-mm slice thickness and 3-or 5-mm reconstruction interval were used. Parameters of above scanning include 120 kV and 150 to 200 mA. | |||||||
For dedicated evaluation of the pancreas, after fasting for at least 2 to 3 hours, each patient ingested 750 to 1000 mL of water. Typically, we administer 500 to 750 mL of water 20 to 30 minutes before the study and an additional 250 mL of water immediately before the study. We injected 100 to 120 mL of iohexol (Omnipaque 350; GE Healthcare, Princeton, NJ) through the peripheral venous line at 3 to 4 mL/s. We acquire dual phase imaging at 25 seconds for arterial phase and 55 to 60 seconds for early portal venous phase from the start of an intravenous contrast material. | |||||||
For multiplanar reformation imaging, image data were reconstructed with the body soft tissue algorithm and sent to a workstation (Leonardo, Siemens Medical Solutions). InSpace software (Siemens Medical Solutions) was used for data analysis that was the volume imaging application for interactive viewing of volume data available on the Leonardo workstation. The images were reviewed using real-time scrolling and interactive multiplanar techniques. | |||||||
CT APPEARANCE OF FOCAL FATTY INFILTRATION OF THE PANCREAS | |||||||
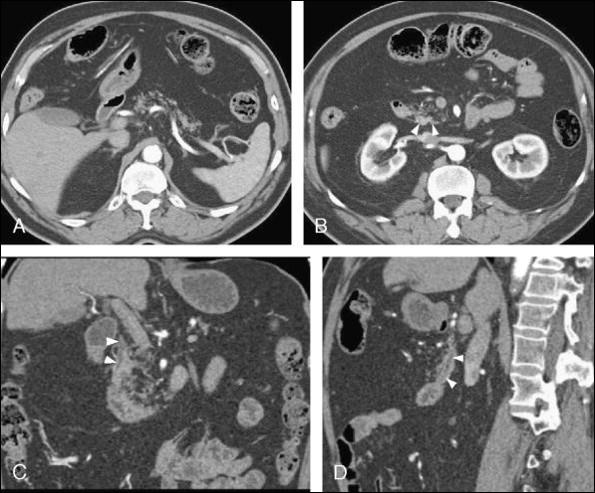
When fatty infiltration involves the pancreas diffusely, it is seen on CT as separation of the parenchymal tissue by intermixed fat diffusely involving the entire pancreas (Fig. 1).1 The individual lobules of the pancreatic parenchyma become more apparent separated by hypoattenuating fat.1 In more pronounced examples, fat becomes the predominant tissue of the pancreas.1 Fat attenuation is usually easily detected by measurement of CT attenuation.4 The size and morphology of the pancreas is often maintained; however, the size of the pancreas may be reduced (Fig. 1) or enlarged. | |||||||
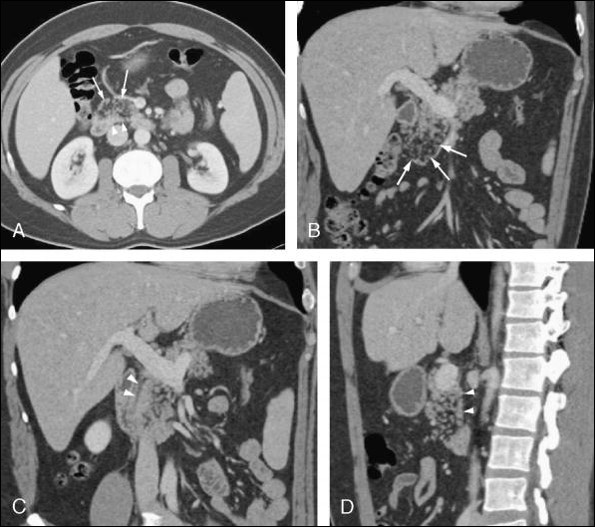
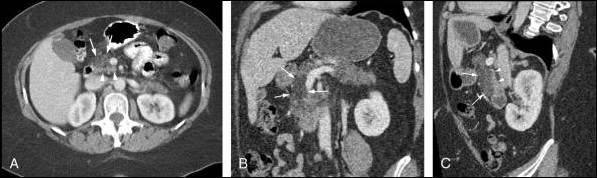
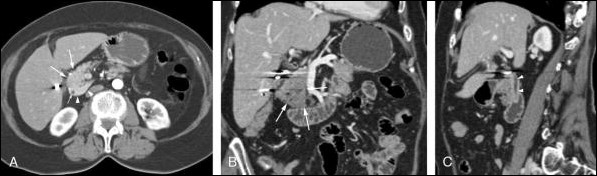
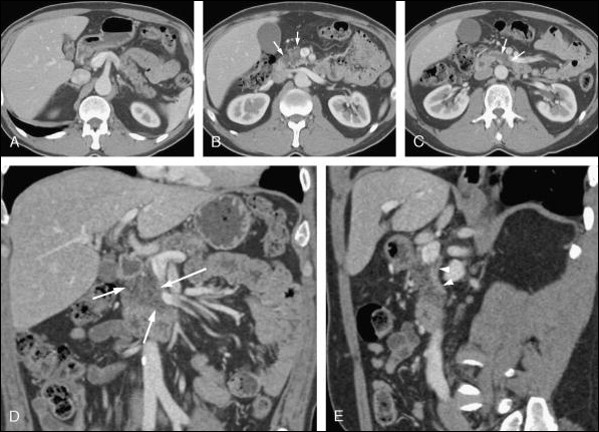
Focal fatty infiltration is often most prominent in the anterior aspect of the head of the pancreas, whereas the posterior aspect of the head of the pancreas and the area around the common bile duct tend to be spared (Figs. 2-6).5,10,11 Focal fatty infiltration is often stable on follow-up CT examination 10; however, the extent of involvement may progresson serial scans.11 | |||||||
Matsumoto et al 10 reviewed CT scans of 1000 cases and found that 3.2% of patients had uneven fatty infiltration. They evaluated 80 patients with uneven fatty infiltration of the pancreas on CT and classified uneven fatty infiltration into 2 types: in type 1, there is uneven fatty infiltration in the head of the pancreas with sparing of the posterior aspect of the head and uncinate process of the pancreas. In type 2, there is uneven fatty infiltration in the head and uncinate process of the pancreas with the focal area of sparing only around the common bile duct. They reported that 57 of the 80 patients (71%) had type 1 fatty infiltration, and 23 patients (29%) had type 2.10 Each type was further divided into 2 subgroups on the basis of whether or not the body and tail of the pancreas showed intense fatty infiltration. Among the 57 patients with type 1 fatty infiltration, 28 patients (35%) had fatty infiltration in the body and tail, and 29 (36%) did not have fatty replacement in the body and tail. Among the 23 patients with type 2 fatty replacement, 9 (11%) had fatty infiltration in the body and tail, and 14 (18%) did not have fatty infiltration in the body and tail.10 In all patients with uneven fatty infiltration, the anterior aspect of the head of the pancreas was involved with fatty infiltration, and the area around the common bile duct was spared in this study.10 They also reported that anteroposterior diameter of the head of the pancreas in patients with intense fatty infiltration is larger than that of control group.10 Massive enlargement of the pancreas caused by intense fatty infiltration is known as lipomatous pseudohypertrophy.1 | |||||||
Focal fatty infiltration in the pancreas is seen as a region of decreased attenuation in the pancreas on noncontrastor postcontrast CT (Figs. 2-6).7 Computed tomographic attenuation within the focal fatty infiltration may be negative and show apparent fat attenuation.10 In these cases, diagnosis of focal fatty infiltration can be supported by measuring CT attenuation (Fig. 2). However, when focal fatty infiltration is mild, the region may not show apparent fat attenuation and may simulate a hypoattenuating mass on CT.8 In such cases, differentiation of tumor and focal fatty infiltration can be difficult. | |||||||
On CT, the area of focal sparing of fatty infiltration is typically seen as a platelike 10 or triangular area 11 of higher attenuation in the posterior part of the pancreatic head and in the uncinate process, in contrast to the anterior aspect of the pancreatic head where there is focal fatty infiltration (Figs. 1-6). The pancreas parenchyma surrounding the common bile duct is often spared,5,10 and it is well visualized on axial and reformation imaging (Figs. 1, 2, 4). However, focal fatty spearing has been reported to be seen as a rounded hyperattenuating area relative to the fatty infiltrated pancreas on contrast-enhanced CT and can mimic a mass.11 | |||||||
The interface between focal fatty infiltration in the anterior aspect of the head of the pancreas and focal area of fatty sparing in the posterior aspect often has a smooth, distinct border on axial- or sagittal-reformatted images (Figs. 1-6). Similar findings were also reported by ultrasound. The area offocal fatty sparing is seen as the hypoechoic zone with sharp margin with anterior aspect of the pancreatic head, and the common bile duct is often seen within this hypoechoiczone on both the transverse and sagittal views by ultrasound.5 The area of intense fatty infiltration in the pancreatic head may gradually change to less intense fatty infiltration in the body and tail of the pancreas, and can be seen as ageographic area of hypoattenuation on axial or coronal reformations. In our experience, the hypoattenuating portion of the pancreas due to focal fatty infiltration usually extends to the anterior and inferior surface of the pancreatic head, maintaining normal contour of the pancreas (Figs. 3-6). | |||||||
CT FINDINGS TO HELP DIFFERENTIATE FOCAL FATTY INFILTRATION FROM PANCREATIC NEOPLASM | |||||||
On CT, the area of hypoattenuation by focal fatty infiltration preserves the normal pancreatic contour and lobular appearance of the parenchyma.10 There are no associated features of malignancy; for example, the pancreatic and bile ducts are not dilated, the adjacent vessels are not displaced orinvaded, and there is no associated adenopathy in patients with focal fatty infiltration.7,8,11 The sharp interface from the embryological ventral pancreas that extends in the craniocaudal direction, well visualized on sagittal-reformatted CT images, also helps to distinguish focal fatty infiltration from apathologic process.5 The uncinate process maintains its normal configuration in patients with focal fatty sparing.11 However, in some cases, it is difficult or impossible to differentiate focal fatty infiltration from a non-border-deforming neoplasm of the pancreas on CT.11 | |||||||
THE USEFULNESS OF MRI TO CHARACTERIZE FOCAL FATTY INFILTRATION | |||||||
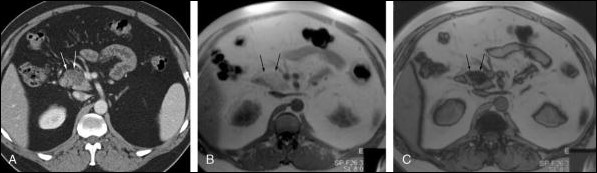
Computed tomography is accurate in detecting macroscopic fat. However, for lesions containing both fatty and nonfatty tissue within a voxel, CT is less accurate in revealing microscopic fat deposits.8 For focal nodular fatty infiltration of the liver, MRI, including a combination of in-phase and opposed-phase gradient-echo imaging, can reliably differentiate focal fatty infiltration from malignancy.25-27 Isserow et al 8 reported that MRI using chemical shift technique can detect and characterize focal fatty infiltration of the pancreas and exclude a diagnosis of neoplasm. On MRI, regions of focal fatty infiltration are isointense to hyperintenseregion relative to the surrounding pancreatic parenchyma on in-phase T1-weighted gradient-echo images, and these regions show moderate to marked signal intensity loss on opposed-phase gradient-echo images (Fig. 6).8 In patients with focal fatty sparing, MRI may also be helpful to exclude the presence of neoplasm by the lack of a hypointense lesion on T1-weighted imaging with normal appearance on T2-weighted images.8,11 | |||||||
CONCLUSIONS | |||||||
Focal fatty infiltration is often seen in the anterior aspect of the head of the pancreas and often spares the dorsal aspect of the head and uncinate process. When apparent fat attenuation is seen on CT, it can be differentiated from a pancreatic neoplasm without difficulty. Focal fatty infiltration does not cause associated features of malignancy; for example, it preserves the normal pancreatic contour and lobule-like appearance of the parenchyma, and the pancreatic and biliary ducts are not dilated. The sharp demarcation from the embryological ventral pancreas that is well visualized on axial- orsagittal-reformatted images also helps to distinguish focal fatty infiltration from a pathological process. However, in some cases, it can be difficult or impossible to differentiate focal fatty infiltration from a non-border-deforming neoplasm of the pancreas on CT. In such cases, MRI using chemical shift technique can be performed to establish the lipid content of the focal abnormality and exclude a diagnosis of neoplasm. | |||||||
REFERENCES | |||||||
1. Katz DS, Hines J, Math KR, et al. Using CT to reveal fat-containing abnormalities of the pancreas. AJR Am J Roentgenol. 1999;172:393-396. | |||||||
2. Walters MN. Adipose atrophy of the exocrine pancreas. J Pathol Bacteriol. 1966;92:547-557. | |||||||
3. Olsen TS. Lipomatosis of the pancreas in autopsy material and its relation to age and overweight. Acta Pathol Microbiol Scand [A]. 1978;86A:367-373. | |||||||
4. Patel S, Bellon EM, Haaga J, et al. Fat replacement of the exocrine pancreas. AJR Am J Roentgenol. 1980;135:843-845. | |||||||
5. Atri M, Nazarnia S, Mehio A, et al. Hypoechogenic embryologic ventral aspect of the head and uncinate process of the pancreas: in vitro correlation of US with histopathologic findings. Radiology. 1994;190:441-444. | |||||||
6. Donald JJ, Shorvon PJ, Lees WR. A hypoechoic area within the head of the pancreas-a normal variant. Clin Radiol. 1990;41:337-338. | |||||||
7. Hague J, Amin Z. Focal pancreatic lesion: can a neoplasm be confidently excluded? Br J Radiol. 2006;79:627-629. | |||||||
8. Isserow JA, Siegelman ES, Mammone J. Focal fatty infiltration of the pancreas: MR characterization with chemical shift imaging. AJR Am J Roentgenol. 1999;173:1263-1265. | |||||||
9. Marchal G, Verbeken E, Van Steenbergen W, et al. Uneven lipomatosis: a pitfall in pancreatic sonography. Gastrointest Radiol. 1989;14:233-237. | |||||||
10. Matsumoto S, Mori H, Miyake H, et al. Uneven fatty replacement of the pancreas: evaluation with CT. Radiology. 1995;194:453-458. | |||||||
11. Jacobs JE, Coleman BG, Arger PH, et al. Pancreatic sparing of focal fatty infiltration. Radiology. 1994;190:437-439. | |||||||
12. Silverman PM, McVay L, Zeman RK, et al. Pancreatic pseudotumor in pancreas divisum: CT characteristics. J Comput Assist Tomogr. 1989;13:140-141. | |||||||
13. Lozano M, Navarro S, Perez-Ayuso R, et al. Lipomatosis of the pancreas: an unusual cause of massive steatorrhea. Pancreas. 1988;3:580-582. | |||||||
14. Dreiling DA, Elsbach P, Schaffner F, et al. The effect of restriction of protein and total calories on pancreatic function in obese patients. Gastroenterology. 1962;42:686-690. | |||||||
15. Tham RT, Heyerman HG, Falke TH, et al. Cystic fibrosis: MR imaging of the pancreas. Radiology. 1991;179:183-186. | |||||||
16. Soyer P, Spelle L, Pelage JP, et al. Cystic fibrosis in adolescents and adults: fatty replacement of the pancreas-CT evaluation and functional correlation. Radiology. 1999;210:611-615. | |||||||
17. Vaughn DD, Jabra AA, Fishman EK. Pancreatic disease in children and young adults: evaluation with CT. Radiographics. 1998;18:1171-1187. | |||||||
18. Uchida T, Takada T, Ammori BJ, et al. Three-dimensional reconstruction of the ventral and dorsal pancreas: a new insight into anatomy and embryonic development. J Hepatobiliary Pancreat Surg. 1999;6:176-180. | |||||||
19. Suda K, Mizuguchi K, Hoshino A. Differences of the ventral and dorsal anlagen of pancreas after fusion. Acta Pathol Jpn. 1981;31:583-589. | |||||||
20. Orci L, Stefan Y, Malaisse-Lagae F, et al. Pancreatic fat. N Engl J Med. 1979;301:1292. | |||||||
21. Dhillon AP, Rode J, Lowers JR, et al. Morphologic distinction of ventral and dorsal analgen in adult pancreas (abstr). J Pathol. 1985;146:263-264. | |||||||
22. Cohen DJ, Fagelman D. Pancreas islet cell carcinoma with complete fatty replacement: CT characteristics. J Comput Assist Tomogr. 1986;10:1050-1051. | |||||||
23. Toyama N, Kamiyama H, Suminaga Y, et al. Pancreas head carcinoma with total fat replacement of the dorsal exocrine pancreas. J Gastroenterol. 2004;39:76-80. | |||||||
24. Maeda H. [Ductal and vascular factors in the etiology of experimentally induced pancreatic fibrosis and fat replacement in dogs]. Nippon Shokakibyo Gakkai Zasshi. 1986;83:2580-2587. | |||||||
25. Kroncke TJ, Taupitz M, Kivelitz D, et al. Multifocal nodular fatty infiltration of the liver mimicking metastatic disease on CT: imaging findings and diagnosis using MR imaging. Eur Radiol. 2000;10:1095-1100. | |||||||
26. Merkle EM, Nelson RC. Dual gradient-echo in-phase and opposed-phase hepatic MR imaging: a useful tool for evaluating more than fatty infiltration or fatty sparing. Radiographics. 2006;26:1409-1418. | |||||||
27. Hussain SM, Zondervan PE, IJzermans JN, et al. Benign versus malignant hepatic nodules: MR imaging findings with pathologic correlation. Radiographics. 2002;22:1023-1036; discussion 1037-1029. | |||||||
Key Words: pancreas; focal fatty infiltration; multidetector CT; multiplanar reformation imaging | |||||||
IMAGE GALLERY | |||||||